Hand Infections Treatment Specialist in Houston, TX
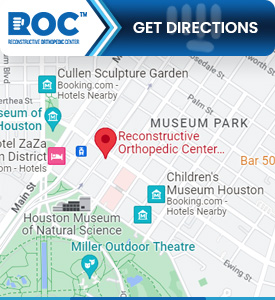
Common questions asked by patients: What is the most common hand infection? What does infected hand look like? How do you treat an infected hand? What are the early signs of hand infection? If you are looking for a hand infection treatment specialist please visit Reconstructive Orthopedic Center in Houston, TX. For more information, contact us today or schedule an appointment online. We are conveniently located at 1200 Binz St #100, Houston, TX 77004. We serve patients from Houston TX, Midtown TX, Montrose TX, MacGregor TX, South Central Houston TX, Old Braeswood TX, and surrounding areas.




Additional Services You May Need
- Injuries
- Orthopedic Surgery
- Same-Day Surgery
- Sports Medicine
- On-call 24 Hours
- Walk-in Patients
- Hands
- Wrist
- Shoulder Surgery
- Foot & Ankle
- Knee
- Physical Therapy
- Occupation Therapy
- Formal Hand Therapy
- Drug Testing
- Tetanus Shots
- Evaluation
- Casting
- Minor Laceration
- Splinting
- Workers’ Comp Clinic
- Elbow Surgery
- Orthopedic Injury
- Shoulder Injury
- Trauma Care
- Elbow Injury